Systemic Antifungals and Common Interactions
Dermatophytes are a common cause of fungal infections, and clinicians typically treat these infections with topical antifungal creams, lotions, ointments, and powders.
Fungal infections such as tinea capitis, tinea
corporis, and tinea pedis, stem from a dermatophyte infection.
1
Dermatophytes have been studied since 1841
2
and are a common cause of fungal infections.
1
Clinicians typically treat these infections with topical antifungal creams, lotions, ointments, and powders. When using topical antifungal drugs, patients must be aware of common adverse effects (AEs), such as application site irritation and hypersensitivity reactions. These AEs are rarely systemic.
When patients fail to respond to topical therapy or have extensive skin involvement, they may need an oral antifungal agent. Systemic antifungals, however, increase the need to consider drug interactions.
Many oral antifungal options belong to the
azole family, including fluconazole, isavuconazole, itraconazole, ketoconazole, miconazole, posacon- azole, and voriconazole.
3
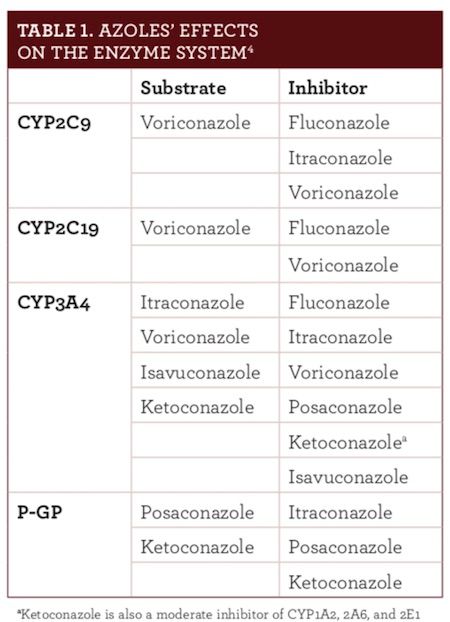
Azoles destroy fungi by inhibiting conversion of lanosterol to ergosterol by the CYP450 enzyme system.
3
Unfortunately, the enzyme inhibition that makes these drugs effective also results in most of the AEs and drug interactions. As noted in Table 1
,
4
azole antifungals inhibit CYP2C9, CYP2C19, CYP3A4, or P-GP. CYP3A is the largest fraction of the total human CYP enzyme content, making many drugs susceptible to interactions.
4
STATIN INTERACTIONS
The azoles’ inhibitory actions affect many commonly used statins.
3
Taken concomitantly with statins, azoles increase the potential for statin-associated myopathy (SAM), which can range from insignificant myalgia to rhabdomyolysis.
5
The 2 most significant azole-statin interactions involve ketoconazole and posaconazole. Strong CYP3A4 inhibitors, they can increase statin concentration about 10-fold.
3
Ketoconazole and posaconazole are contraindicated for use with statins metabolized via CYP3A4.
3
If posaconazole is prescribed for patients taking atorvastatin, lovastatin, or simvastatin, the statin must be held until the antifungal treatment is complete.
3
Then, upon restarting the statin, clinicians should continue to monitor patients for SAM, as posaconazole’s half-life ranges from 24 to 30 hours.
3
Pravastatin and rosuvastatin are least likely to be affected by azoles because they have limited CYP450 metabolism. Ketoconazole also inhibits the OATP1B1 transporter, which can increase pravastatin and rosuvastatin levels.
3
Therefore, prescribers should use ketoconazole cautiously with these 2 drugs.
3
IMMUNOSUPPRESSANT INTERACTIONS
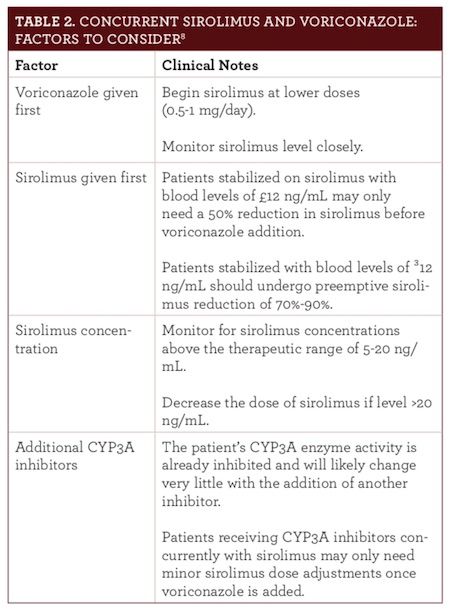
Azoles and immunosuppressants also interact. Voriconazole can increase sirolimus levels from 7- to 11-fold,
6
and posaconazole can increase sirolimus levels about 9-fold.
7
Both drugs are con- traindicated for use with sirolimus.
6,7
However, these drugs can be given concurrently when necessary (Table 2
).
8
Doing so requires a sirolimus dose reduction up to 90%, careful consideration of which drug is given first, sirolimus concentration, concurrent disease states, and additional CYP3A inhibitors.
8
Concentrations of the calcineurin inhibitors, cyclosporine, and tacrolimus, also increase when administered with posaconazole or voriconazole. Prescribers should reduce the original tacrolimus dose by one-third and monitor blood levels frequently when administering it concomitantly with either azole.
6,7
The cyclosporine dose must be reduced by 25% with posaconazole and 50% with voriconazole.
GASTROINTESTINAL EFFECTS ON AZOLE CONCENTRATIONS
Food and gastric pH levels are another consideration.
4
Food lowers absorption of itraconazole and voriconazole, so these drugs must be taken 1 hour before or 1 hour after meals. Conversely, when posaconazole is administered with food, its absorption increases.
4
Therefore, clinicians should instruct patients to take this medication within 20 minutes following a meal.
7
Food does not affect fluconazole’s absorption, so it may be taken without regard to meals.
9
It is also essential for providers to ask if patients are taking OTC or prescription H
2
receptor antagonists (H
2
RA) or proton pump inhibitors (PPI). When itraconazole or posaconazole are taken with H
2
RAs or PPIs, antifungal absorption can be impaired, leading to subtherapeutic drug levels.
4
Finally, azoles can prolong the QTc interval, elevating the risk for torsade de pointes.
10
Although this adverse event is important in its own right, it is more likely when azoles are taken concomitantly with a number of other medications. The azoles/fluoroquinolone combination is particularly interesting. Commonly prescribed in patients with hematology as prophylaxis, these drugs address bacterial and fungal infections.
11
Both drugs can prolong the QTc interval and increase the risk of torsades de pointes synergistically if given together.
11
Clinicians with patients on this combination should monitor each patient’s QTc interval closely.
And remember: Just because a patient takes an antifungal drug
does not mean that drug is being used to treat a fungal infection. For example, ketoconazole has an off-label use in advanced cases of prostate cancer
12
and in Cushing syndrome to help reduce cortisol levels.
13
CLINICIANS IN PRACTICE
This summary mentions only a few interactions. Because of the wide range of effects the azoles have on the human body, many more interactions are possible. Clinicians must check for possible drug interactions when patients take oral antifungals.
References
- Seebacher C, Bouchara JP, Mignon B. Updates on the epidemiology of dermatophyte infections.Mycopathologia.2008;166(5-6):335-52. doi: 10.1007/s11046-008-9100-9.
- Gräser Y, Monod M, Bouchara JP, et al. New insights in dermatophyte research.Med Mycol.2018;56(suppl 1):S2-S9. doi: 10.1093/mmy/myx141.
- Hylton Gravatt LA, Flurie RW, Lajthia E, Dixon DL. Clinical guidance for managing statin and antimicrobial drug-drug interactions.Curr Atheroscler Rep.2017;19(11):46. doi: 10.1007/s11883-017-0682-x.
- Brüggemann RJ, Alffenaar JW, Blijlevens NM, et al. Clinical relevance of the pharmacokinetic interactions of azole antifungal drugs with other coadministered agents.Clin Infectious Dis.2009;48(10):1441-1458. doi: 10.1086/598327.
- Vrablik M, Zlatohlavek L, Stulc T, et al. Statin-associated myopathy: from genetic predisposition to clinical management.Physiol Res.2014;63(suppl 3):S327-S334.
- Voriconazole [prescribing information]. New York, NY: Pfizer, Inc; 2010. www.accessdata.fda.gov/drugsatfda_docs/label/2010/021266s032lbl.pdf. Accessed July 2, 2018.
- Posaconazole [prescribing information]. Whitehouse station, NJ: Merck & Co, Inc; 2015. www. accessdata.fda.gov/drugsatfda_docs/label/2015/022003s018s020,0205053s002s004,0205596s001s003lbl.pdf. Accessed July 2, 2018.
- Surowiec D, DePestel DD, Carver PL. Concurrent administration of sirolimus and voriconazole: a pilot study assessing safety and approaches to appropriate management.Pharmacotherapy.2008;28(6):719-729. doi: 10.1592/phco.28.6.719.
- Fluconazole [prescribing information]. New York, NY: Pfizer, Inc; 2011. www.accessdata.fda.gov/drugsatfda_docs/label/2011/019949s051lbl.pdf. Accessed July 2, 2018.
- Salem M, Reichlin T, Fasel D, Leuppi-Taegtmeyer A. Torsade de pointes and systemic azole antifungal agents: analysis of global spontaneous safety reports.Global Cardiol Sci Pract.2017(2):11. doi: 10.21542/gcsp.2017.
- Zeuli JD, Wilson JW, Estes LL. Effect of combined fluoroquinolone and azole use on QT prolongation in hematology patients.Antimicrob Agents Chemother.2013;57(3):1121-1127. doi: 10.1128/AAC.00958-12.
- Harris KA, Weinberg V, Bok RA, Kakefuda M, Small EJ. Low dose ketoconazole with replacement doses of hydrocortisone in patients with progressive androgen independent prostate cancer.J Urol.2002;168(2):542-545.
- Castinetti F, Guignat L, Giraud P, et al. Ketoconazole in Cushing's disease: is it worth a try?J Clin Endocrinol Metab.2014;99(5):1623-1630. doi: 10.1210/jc.2013-3628.