Anal Itching, Hemorrhoids, Leakage, Warts: Benign but Agonizing
Over the last few years, several journals have published articles about anal healthcare.
Over the last few years, several journals have published articles about anal healthcare. Almost exclusively, the authors indicate that primary care providers often have little understanding of the most frequent problems that occur around the anal sphincter. In addition, patients often think they simply have a hemorrhoid (which accounts for less than half of anal problems) and frequently hesitate to mention these problems, suffering in silence because of unnecessary modesty or due to perceived stigma. Reviewing common complaints and differential diagnosis can increase competence in this area.
Common Complaints
Patients who are experiencing problems associated with their anal sphincters usually present with four possible primary symptoms: itching, pain, discomfort, or bleeding. Retail healthcare providers need to determine the symptoms' etiology, provide effective treatment strategies, and determine if patients need follow-up or additional evaluation. Fortunately, most anal problems are benign.
As always, assessment begins with a history, and retail healthcare practitioners will need to ask about bowel frequency, quality and consistency of the bowel movement, and length of time patients spend on the toilet (and whether they engage in distracting activities like reading or playing games while on the toilet). It's also important to ask patients describe the symptoms, their anal self-care routine, and of course, their diet and the amount of fiber in it.
Physical Exam
During visual examination, retail healthcare providers need to look for signs of acute or chronic irritation. Since cleansing products can be allergens and irritants, it's important to look for signs of contact dermatitis, thrombosed hemorrhoid with or without ulceration, and external fistula openings. Some patients who have histories of hemorrhoids develop anal skin tags, and patients who have fistulas sometimes develop skin tags adjacent to the fistula opening.
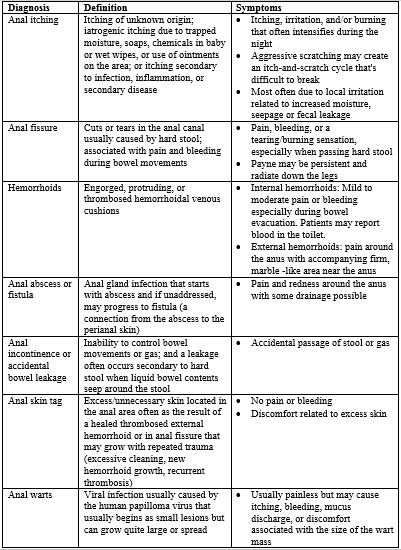
Table 1 differentiates between the most common seven diagnoses.
Table 1. Common Anal Diagnoses
Treatment
Regardless of the patient's complaint, retail healthcare providers need to assess the patient's fiber intake and ensure that it's adequate. Each patient's daily intake goal should be 25 to 40 g of fiber. Adequate fiber regulates bowel movements, softens hard stool, and reduces risk of colon and rectal cancer and diverticulosis. It can also lower cholesterol. The best source of fiber is dietary, and retail healthcare providers may need to educate patients about how to find each food's fiber content on its label. Fresh fruits and vegetables are not ribald but numerous websites are available to help patients identify fiber content. Advise patients who consume little fiber to increase their fiber content gradually by 5 g of fiber each week until they reach goal. Patients who increase their fiber to quickly are likely to develop excessive gas. Also recommend fiber supplements and increasing water to 8 to 10 glasses daily.
By the time most patients seek help, they will have tried a number of over-the-counter interventions. Ask patients about these interventions, and warn them that they often unintentionally exacerbate the problem. Hemorrhoidal creams, especially those that contain steroids, can help in the short-term, but steroids contribute to skin atrophy and use should be limited to two weeks. Ointments containing zinc oxide are the safest alternative for anal complaints.
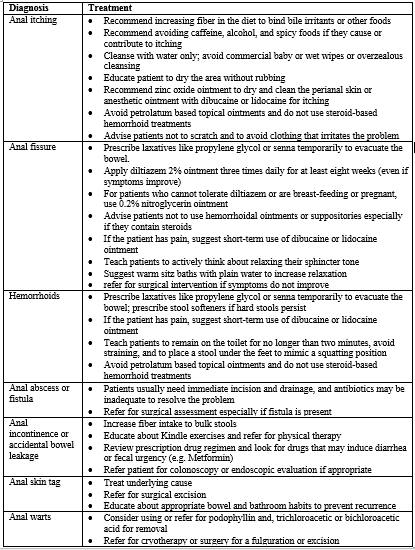
Table 2. Simple Treatment Approaches to Anal Complaints
Conclusion
Some patients will need systemic treatment for pain or itching. Usually, standard doses of acetaminophen or nonsteroidal anti-inflammatory drugs can reduce pain to tolerable levels. Using a sedative antihistamine at bedtime can reduce the urge to scratch during the night.
Sources
Ansar P. Pruritis Ani. Clin Colon Rectal Surg. 2016;29:38-42.
Chang J, McLemore E, Tejirian T. Anal Health Care Basics. Perm J. 2016_20(4):15-22. Available at http://www.thepermanentejournal.org/files/Fall2016/AnalHemorroids.pdf. Accessed June 30, 2017.
Wald A; Bharucha AE; Cosman BC; Whitehead WE. ACG clinical guideline: management of benign anorectal disorders. Am J Gastroenterol. 2014; 109(8):1141-57.
