The ICD-10 Transition: What You Need to Know
One of the basic tenets that will remain constant in the transition from ICD-9 to ICD-10 is the role of clinical documentation.
One of the basic tenets that will remain constant in the transition from ICD-9 to ICD-10 is the role of clinical documentation.
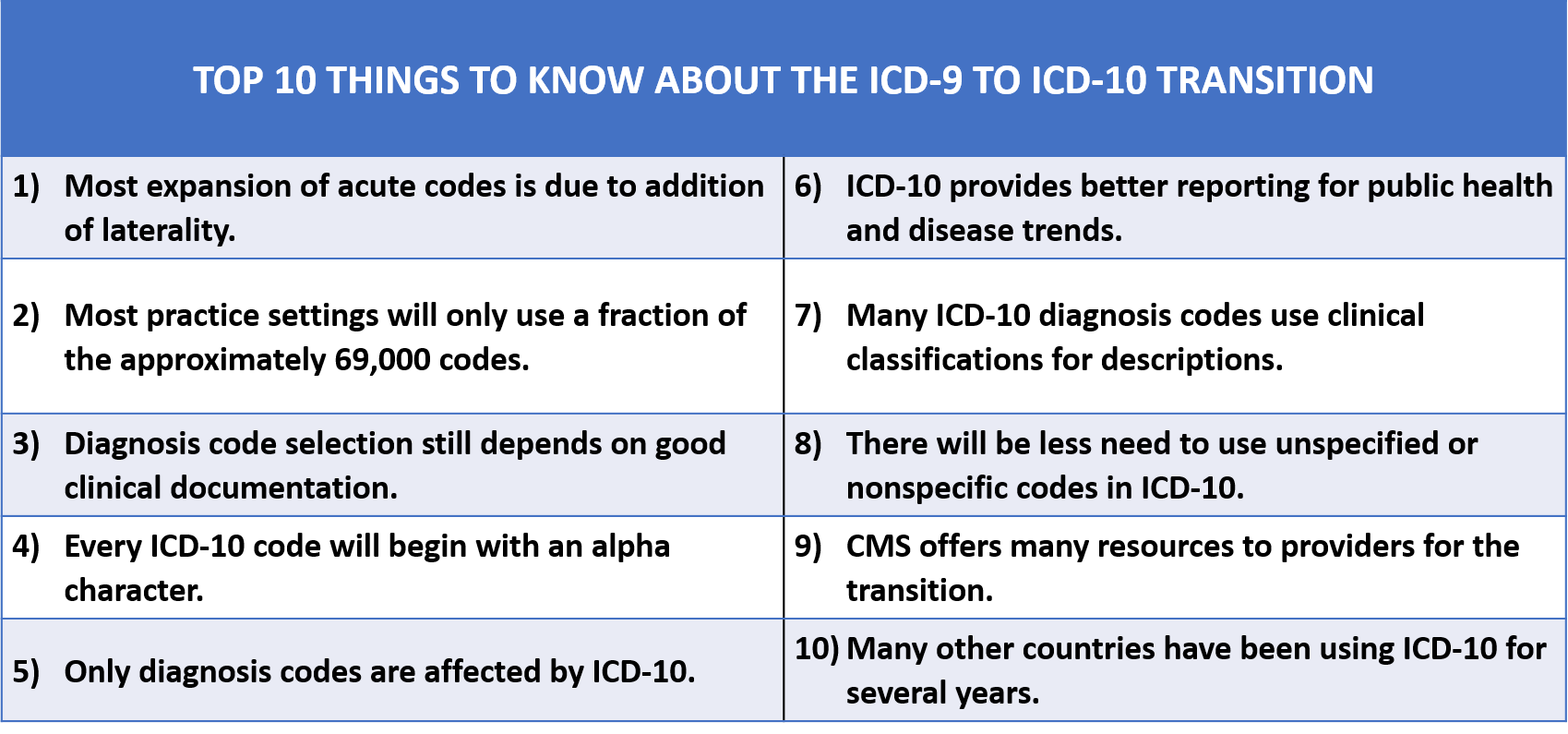
After several delays, the United States implemented International Classification of Diseases, 10th Revision, Clinical Modification, also known as ICD-10, on October 1, 2015. This is a federal mandate that affects every health care provider in the United States. Australia was the first country to employ this update to its clinical cataloging system and the United States is the last country to adopt ICD-10 coding. ICD-10 will provide the ability to more accurately represent disease conditions and their severity and is expected to positively impact reporting of patient status, research, and public health trends. Understanding the benefits of the transition to ICD-10 in addition to its similarities with ICD-9 will alleviate much of the apprehension felt by most providers.
Clinical Documentation Matters
One of the basic tenets that will remain constant in the transition from ICD-9 to ICD-10 is the role of clinical documentation. The Centers for Medicare & Medicaid Services (CMS) guidelines for coding will not change with the transition, and the diagnosis code(s) assigned to a patient encounter will continue to require validation by the information in the medical record. With the transition to ICD-10, providers may need to become more familiar with documentation requirements for clinical classification of disease groupings. For example, asthma is one category in ICD-10 that has changed its code descriptions to align with its clinical classification. The clinical classification of asthma now includes specific terminology to reflect mild, moderate, or severe, and whether the condition is intermittent or persistent. Therefore, documentation should support the severity of the asthma with findings in the history of present illness or a review of systems to demonstrate frequency of symptoms and/or frequency of inhaler use. Since many categories of ICD-10 diagnosis codes rely on clinical classification, if it cannot be easily inferred from the documentation, a provider’s ability to identify the most accurate and specific diagnosis code may be limited.1
For other conditions, a patient’s past medical history may be an important piece of supporting documentation. If there is information in the medical history to support the etiology, manifestation, or complication associated with a disease, this information needs to be pulled forward into the encounter note. Conditions listed in the chart but not validated for the present encounter cannot be considered as supporting documentation; selecting them in the encounter note demonstrates validation of the current status since many conditions on a past-history list may resolve or progress and worsen.
ICD-10 Code Selection
ICD-10 has a more logical grouping of code categories and follows the ICD- 9 classification principles to arrange codes primarily by anatomy, etiology, or type of disease. An enhancement in ICD-10 is the categorizing of eye and ear disorders into their own chapters to make identification of these codes simpler. There are several coding resources available to assist providers in searching for the desired ICD-10 code. Available resources include coding books, search engines, apps, and electronic health record-embedded search engines. Each tool has its own list of pros and cons, so individual preference should be considered for ease of use. Providers should identify their preferred search tool as early as possible and practice using it frequently to become proficient in searching for the appropriate ICD-10 code.
Coding rules for ICD-10 have changed slightly from ICD-9, and the complete set of chapter-specific rules continues to be published by CMS. PDF document can be found on the CMS website.2Many of the ear, nose, and throat—related acute conditions and several chronic disease categories have coding rules for circumstances such as tobacco use and exposure. Many commercial electronic health records have these rules embedded within their systems to better assist the provider in correct code selection and proper sequencing of the diagnosis codes. However, providers are still advised to become familiar with the common coding rules associated with the diagnosis codes used most frequently in their area of practice.
Unspecified Codes in ICD-10
The increase in specificity for the majority of codes in ICD-10 will minimize the need to use nonspecific or unspecified codes. CMS has issued a directive for ICD-10 that provides guidance on the leniency it will grant for the first year of ICD-10 implementation regarding the use of less-specific code assignment by providers. This directive by CMS indicates that as long as a provider has selected a valid code from an appropriate code family, it will accept the code even if it is not the most specific.3There are inherent risks with this guidance. First, if providers choose to adopt this leniency, they may be setting themselves up for failure. If they get into the practice of using less-than-desirable code selection, they will have to change this pattern of behavior once the grace period has expired. Also, this directive is only issued by CMS and does not apply to any of the commercial payers, so providers could find themselves with claims not being accepted by commercial payers due to their code selection.
There are 2 main designations for unspecified codes that will remain unchanged from ICD-9 to ICD-10. These designations are NOS (not otherwise specified) and NEC (not elsewhere classified). The primary difference between the 2 codes is the role of documentation. When a code is selected with an NOS indicator, this shows that the documentation does not support a more specific diagnosis code. Before assigning an NOS code to an encounter, it is important to review the documentation to ensure that a more specific match cannot be made or to determine whether there are elements of documentation omitted that need to be included for a more specific selection. If an NEC code is assigned, this means that the documentation was sufficient, but a more specific diagnosis code does not exist to match the documentation. There are fewer NEC codes in ICD-10, and of the two, NOS is the actual unspecified code classification.
Acute Versus Chronic Diagnosis Codes
The expansion impact on acute and chronic diagnosis codes for ICD-10 allow for more accurate report of conditions. The majority of acute disease codes have expanded to allow for laterality, encounter type, and anatomic details. For example, eye and ear disorder codes allow the provider to code for the specific affected side with the addition of right, left, and bilateral designations. In addition, eye disorders can be specified to the exact eyelid affected, upper and lower.
Chronic disease codes in ICD-10 will also allow for better capture of severity, complications, and manifestations. Key chronic conditions such as hypertension or diabetes will also have combination codes to allow for a more accurate representation of disease severity. Documentation requirements will remain unchanged, so the provider will need to focus on key elements in both the history and physical exam to support combination codes for chronic conditions that include either manifestations or complications of a disease.
Many chronic disease codes have coding rules for underlying conditions and complications. For example, when diagnosing a patient with diabetes with kidney disease, it is necessary to add an additional diagnosis code for the stage of kidney disease. If lab values are not readily available and the patient is unsure of their staging, it would still be appropriate to add the diagnosis code for the unspecified stage of kidney disease.4
Remember the Basics
Two key elements that support diagnosis code selection are good clinical documentation and medical necessity. This will remain unchanged in the transition from ICD-9 to ICD-10. Documentation should accurately reflect both the level of work for the care rendered and support the selected diagnosis codes. Over- or under-documentation will result in either incorrect diagnosis code selection or missed diagnosis codes that should have been included. Diagnosis codes should always be selected for the highest level of specificity known about the patient at the time of the encounter.
Medical necessity will always remain the cornerstone in guiding patient care. CMS continues to give clear guidance on medical necessity as the overarching criterion for payment.5Additional testing performed and diagnosis codes assigned should have a direct correlation with the quality and accuracy of the documentation; volume of documentation does not always support medical necessity. Remember that all diagnosis codes assigned to an encounter should reflect the care delivered, and every diagnosis code must have an appropriate treatment plan in order to be billable. (For a quick refresher of the points mentioned previously, review theTop 10 Things to Know About the ICD-9 to ICD-10 Transition.)
ICD-10 Implications for Practice
Now is a good time to do an inventory of pertinent materials used for your clinical practice that may need to be updated for ICD-10. Such materials may include marketing tools or advertising vehicles that do not directly impact patient care. Other areas that carry a higher compliance risk are policy and procedures, patient education materials, and billing forms. In addition, providers should become familiar with the crossover of the diagnosis codes from ICD-9 to ICD-10 that will be used frequently in their patient encounters. One area of impact with the transition could be a reduction in provider efficiency in identifying the correct ICD- 10 diagnosis code, resulting in longer exam times. Longer exam times could result in fewer patients being seen and ultimately impact revenue.6Successful provider preparation is key.
ICD-10 and Claims Submission
Perhaps one of the biggest areas of concern for providers and health care organizations is the potential impact on revenue that ICD-10 may have. Upfront effects such as those discussed previously in this article the responsibility of the provider to mitigate. The next step of the reimbursement process is generating the diagnosis and procedure codes into the appropriate claim transmission for reimbursement. CMS has been offering testing opportunities for the last few years to support the readiness of organizations for claims submission. Each entity is responsible to ensure their billing system is capable of submitting the appropriate ICD-10 diagnosis codes for a date of service on or after October 1, 2015. If the receiving entity has not prepared their system to receive the claim sent, the liability rests on their shoulders for not meeting the requirements of the federal mandate.7
Jennifer Hayes, DNP, FNP-BC, CPC, is a board-certified family nurse practitioner, certified professional coder, and American Health Information Management Association-approved ICD-10 Trainer with over 20 years of combined health care experience. She currently serves as the manager of medical coding for Walgreens Healthcare Clinics, overseeing clinical coding and documentation, coding accuracy, and ICD-10 transition.
References
- Centers for Medicare & Medicaid Services. ICD-10: the road forward. CMS website. www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNGenInfo/downloads/PR-ICD-10.pdf.
- Centers for Medicare & Medicaid Services. ICD-10-CM official guidelines for coding and reporting—FY 2016. CMS website. www.cms.gov/Medicare/Coding/ICD10/Downloads/2016-ICD-10-CM-Guidelines.pdf.
- Centers for Medicare & Medicaid Services. CMS and AMA announce efforts to help providers get ready for ICD-10: frequently asked questions. CMS website. www.cms.gov/Medicare/Coding/ICD10/Downloads/ICD-10-guidance.pdf.
- Centers for Medicare & Medicaid Services. ICD-10 basics. CMS website. www.roadto10.org/icd-10-basics. Published 2014.
- Centers for Medicare & Medicaid Services. Pub 100-04: Medicare claims processing. www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/Downloads/R3315CP.pdf. Published August 6, 2015.
- McCarty J. 10 steps to ICD-10.ASHA Lead. 2014;19(3):36-37. doi: 10.1044/leader.IPP.19032014.36.
- Colpas P. Ensuring a successful ICD-10 conversion.Health Manag Technol. 2013;34(9):8-12.