Avoiding Interactions with Allergy Medications
Allergies are the sixth leading cause of chronic illness in the United States.
Allergies are the sixth leading cause of chronic illness in the United States.1The mainstays of allergy treatment include oral and intranasal antihistamines, decongestants, intranasal corticosteroids (INCs), and leukotriene receptor antagonists.
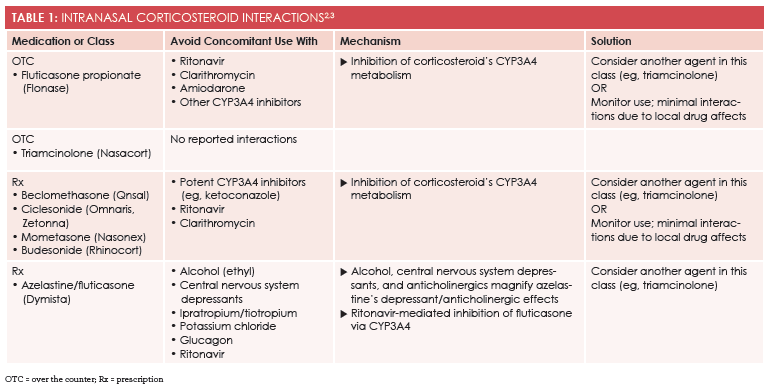
INCs are considered the single most effective class of medications for treating allergic rhinitis (AR) (Table 12,3). Because many patients use OTC medications for seasonal allergies,4however, they may select oral drugs because they are unfamiliar with—and perhaps a little afraid of—INCs. Health care providers are largely responsible for recommending treatment and preventing interactions. In doing so, they can help patients select safe, effective options while advising them on when to step up to prescription drug therapy.
Populations at Risk for Interactions
Monitoring for comorbidities and patient characteristics that elevate the risk for interactions is clever. Two populations that may have more issues with allergy medications than others are the elderly and individuals with hypertension.
The elderly are at elevated risk for interactions because most take multiple medications. This group is also physiologically more sensitive to certain adverse effects (AEs) (eg, drowsiness). The 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults outlines pertinent interactions and potential AEs in the elderly population and serves as a valuable resource for all health care providers.5
Despite their improved AE profile, second-generation antihistamines/intranasal antihistamines, especially cetirizine, may still cause sedation. Elderly patients should be advised to avoid activities that require mental alertness (eg, driving) until they know how their allergy medications could affect them. In addition, elderly men with benign prostatic hyperplasia should avoid pseudoephedrine-containing products and first-generation antihistamines, as these products can further hinder the patient’s ability to urinate.6In terms of patients with hypertension, the decongestants pseudoephedrine and phenylephrine can elevate blood pressure for the duration of use, so those with well-controlled blood pressure may take them with the prescribing provider’s approval.7
Safety of OTC Allergy Medications
Allergy medications represent a rather benign class of remedies. Topical drugs act locally and are devoid of AEs. For the most part, OTC allergy medications are safe and effective when used according to package directions. However, they can pose harm if misused or taken in combination with other OTC and prescription medications.8,9
Because so many allergy medications are OTC remedies, retail health care providers may need to walk down the OTC aisle with patients. Although INCs are most effective and have negligible interactions,4many patients prefer oral drugs. For those with mild AR, the American Academy of Otolaryngology recommends second-generation oral antihistamines (Table 22,3).10
TABLE 2: ORAL AND INTRANASAL ANTIHISTAMINE INTERACTIONS2,3
Medication or Class
Avoid Concomitant Use With
Mechanism
Solution
Oral Antihistamines
OTC
- Fexofenadine (Allegra)
- Fruit juice (grapefruit, orange, apple)
- Aluminum- or magnesium-containing antacids within 30 minutes before/after taking drug
â–ºFruit juice decreases absorption of fexofenadine
â–ºAntacids decrease bioavailability of fexofenadine
Switch to another agent in this class (eg, loratadine)
Wait 30 minutes before taking an antacid
OTC
- Loratadine (Claritin)
- Cetirizine (Zyrtec)
- Azelastine
- Ipratropium
- Tiotropium
- Glucagon
- Potassium chloride
â–º Anticholinergics may enhance similar effects of these agents
â–º Anticholinergics may magnify glucagon’s adverse effects
Consider using an intranasal corticosteroid (eg, mometasone)
Rx
- Desloratadine (Clarinex)
- Levocetirizine (Xyzal)
- Azelastine
- Ipratropium
- Tiotropium
- Glucagon
- Potassium chloride
â–º Anticholinergics may enhance similar effects of these agents
â–º Anticholinergics may magnify glucagon’s adverse effects
Consider using an intranasal corticosteroid (eg, mometasone)
Intranasal Antihistamines
Rx
- Azelastine (Astelin 137 mcg) (Astepro 0.1%) (Astepro 0.15%)
- Olopatadine (Patanase)
- Alcohol (ethyl)
- Central nervous system depressants
- Ipratropium/tiotropium
- Potassium chloride
- Glucagon
â–ºAlcohol/central nervous system depressants and anticholinergics may enhance azelastine’s similar effects
â–º Anticholinergics may magnify glucagon's adverse effects
Consider using an intranasal corticosteroid (eg, mometasone)
Most patients avoid first-generation oral antihistamines (eg, diphenhydramine [Benadryl], chlorpheniramine [Chlor-Trimeton]) because of their propensity to cause drowsiness. However, some patients with severe allergies may find these medications beneficial and will take them at bedtime to relieve symptoms and help them fall asleep. Because patients may experience impairment the following day, they should avoid activities requiring mental alertness (eg, driving) until they know how antihistamines will affect them.11
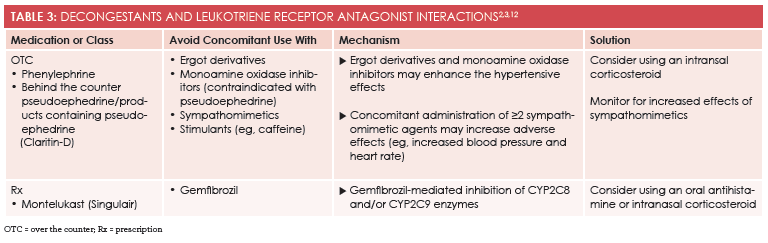
Retail health care providers should also recommend oral decongestants as adjunct therapy when allergies cause congestion and leukotriene receptor antagonists as secondary therapy for patients with comorbid asthma and AR (Table 32,3,12). Products containing phenylephrine are given over the counter, whereas pseudoephedrine products must be purchased at the pharmacy counter. Combination products containing second-generation antihistamines and pseudoephedrine (eg, Claritin-D) have become increasingly popular.
Conclusion
There are abundant medications for AR and accompanying symptoms available, many of which are OTC products. Health care providers should be well versed in treatment options and prepare to provide recommendations and interventions to avoid interactions.
Lauren Crespois a PharmD candidate at the University of Connecticut in Storrs.
References
- Gateway to health communication and social marketing practice: allergies. CDC website. cdc.gov/healthcommunication/toolstemplates/entertainmented/tips/allergies.html. Updated February 2, 2011. Accessed March 11, 2016.
- Lexicomp Online. http://online.lexi.com. Accessed February 17, 2016.
- Micromedex Solutions. http://micromedexsolutions.com. Accessed February 17, 2016.
- American College of Allergy, Asthma & Immunology. Types of allergic rhinitis. ACAAI website. http://acaai.org/allergies/types/hay-fever-rhinitis. Accessed March 11, 2016.
- American Geriatrics Society 2015 Beers Criteria Update Expert Panel. American Geriatrics Society 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults.J Am Geriatr Soc. 2015 Nov;63(11):2227-46. doi: 10.1111/jgs.13702. Epub 2015 Oct 8.
- Cunningham GR, Kadmon D. Patient information: benign prostatic hyperplasia (BPH) (beyond the basics). UpToDate website. uptodate.com/contents/benign-prostatic-hyperplasia-bph-beyond-the-basics. Updated May 28, 2014. Accessed March 11, 2016.
- Coates ML, Rembold CM, Farr BM. Does pseudoephedrine increase blood pressure in patients with controlled hypertension?J Fam Pract. 1995;40(1):22-26.
- Gupta S. OTC drug dangers you should know about. Everyday Health website. everydayhealth.com/news/over-the-counter-drug-dangers-should-know-about/. Published March 20, 2014. Accessed March 11, 2016.
- Understanding over-the-counter medicines. FDA website. fda.gov/Drugs/ResourcesForYou/Consumers/BuyingUsingMedicineSafely/UnderstandingOver-the-CounterMedicines/default.htm. Updated December 16, 2013. Accessed March 11, 2016.
- Seidman M, Gurgel R, Lin S, et al. Clinical practice guideline: allergic rhinitis.Otolaryngol Head Neck Surg.2015;152(1):S1-S43. doi: 10.1177/0194599814561600.
- Casale TB, Blaiss MS, Gelfand E, et al; Antihistamine Impairment Roundtable. First do no harm: managing antihistamine impairment in patients with allergic rhinitis.J Allergy Clin Immunol.2003;111(5):S835-S842.
- Drug interactions: what you should know. FDA website. fda.gov/drugs/resourcesforyou/ucm163354.htm. Updated September 25, 2013. Accessed March 11, 2016.