Safe and Effective Use of Common OTC Analgesics in Convenient Care
Analgesics, particularly acetaminophen and ibuprofen, are among the most commonly used medications in primary care.
Analgesics—particularly acetaminophen and ibuprofen—are among the most commonly used medications in primary care. Indeed, they are often the first-line choice for symptom relief for patients visiting retail clinics.
Even though acetaminophen and ibuprofen are OTC medications, it is vital that practitioners understand how to recommend them properly, especially in conjunction with other medications that may be prescribed. It is equally important to consider the risk-benefit ratio when recommending any medication, including both prescription and nonprescription products.1Knowing the patient’s past and current medical history will assist the practitioner in developing a symptom relief strategy with ibuprofen and/or acetaminophen.
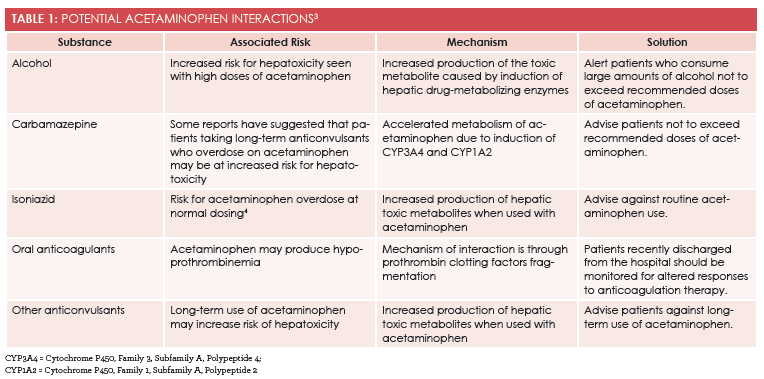
Although the efficacy of alternating ibuprofen and acetaminophen has been questioned, the drugs’ individual safety and efficacy are well proven.1To avoid side effects and unintended consequences from potential interactions, analgesics should be taken at the lowest effective dose for the shortest period of time.2For providers in convenient care settings, the main focus must be 2-fold: immediate relief of the patient’s pain and management of the underlying condition. In order to manage the pain and condition effectively, the practitioner must understand the importance of dose efficacy.Tables 1 and 23provide a reference to potential interactions for both ibuprofen and acetaminophen.
Conclusion
Upon review of the patient’s medication history and any pertinent interactions, it is prudent for the practitioner to review standard OTC dosing for patients. It can be very useful to provide patients with a basic overview of dosing for both acetaminophen and ibuprofen based on the patient’s age and weight. Convenient care practitioners are perfectly situated to provide this level of detailed recommendation for each and every patient to ensure that OTC medication regimens are understood and managed at every clinic visit.
Table 2: Potential Ibuprofen Interactions3
Substance
Associated Risk
Mechanism
Solution
Aspirin
Potential ulcer risk
Interferes with prothrombin coagulation cascade
Advise against concurrent ibuprofen use with aspirin.
Alka-Seltzer
Increased risk for GI ulcers
Interferes with prothrombin coagulation cascade
Advise strict adherence to ibuprofen dosing recommendations.
DMARDs
Increased risk for GI ulcers
Increases sensitivity of prothrombin/thrombin cascade
Advise patient against concurrent ibuprofen use with DMARDs.
Apixaban(Eliquis)
Potential ulcer risk
Interacts with apixaban’s therapeutic dosing regimen and increases sensitivity of prothrombin/thrombin cascade
Advise against concurrent ibuprofen use with apixaban.
Stirbild(elvitegravir, cobicistat, emtricitabine, tenofovir DF)
Potential ulcer risk
Interacts with anticoagulant effects and increases sensitivity of prothrombin/thrombin cascade
Advise against concurrent ibuprofen use with Stribild.
DMARDs = disease-modifying antirheumatic drugs; GI = gastrointestinal; NSAIDs = nonsteroidal anti-inflammatory drugs.
Kristene Digginsis a corporate senior educator at MinuteClinic and faculty member of the University of Phoenix. She has worked as a provider in convenient care for 9 years and enjoys international medical opportunities, as her career goal is to enhance health care access globally.
References
- Moore N, Pollack C, Butkerait P. Adverse drug reactions and drug—drug reactions with over-the-counter NSAIDs.Ther Clin Risk Manag.2015;11:1061-1075.
- Bozimowski G. A review of nonsteroidal anti-inflammatory drugs. AANA J.2015;83(6):425-433.
- Nurses’ guide to O.T.C. analgesics.Nursing93;23(3):66, 68-71, 73-75.
- Murphy R, Swartz R, Watkins PB. Severe acetaminophen toxicity in a patient receiving isoniazid.Ann Intern Med.1990;113(10):799-800. [Correction: Acetaminophen toxicity.Ann Intern Med. 1991;114(11):253.]